Diabetic Foot Conditions
It is estimated that approximately 17 million Americans have diabetes mellitus with almost 1 million new cases diagnosed each year. Diabetes is a multisystem disease that effects the cardiovascular, renal, retinal, nervous and immune systems, which all contribute to diabetic foot complications. Foot ulcers contribute to lower extremity amputations and 85% of diabetes related lower extremity amputations are preceded by a foot ulcer. Routine exams with a foot and ankle specialist is extremely important to prevent ulcerations, infections and amputations.
Causes of diabetic foot complications
- Neurologic Disease

Ten percent of all diabetic patients have some form of sensory, motor, or autonomic dysfunction at the time diabetes mellitus is diagnosed. Sensory neuropathy is the most prevalent nerve dysfunction in diabetic patients and is the major factor precipitating foot ulceration. Pain may be superficial and patients feel a burning, tingling, shooting or cramping/aching type sensation. Motor neuropathy is clinically evident by the presence of claw toes caused my muscle weakness and Achilles tendon contracture. The combination of these factors causes transfers stress leading to high pressures and skin breakdown. Pressure is placed on top of the toes as they come in contact with the toe box of the shoe as well as on the ball of the foot causing a risk of skin breakdown. Autonomic neuropathy occurs when the autonomic nervous system is not able to control the sweat and lubricating glands in the foot causing dryness and cracks in the skin. This allows for a pathway of bacteria to enter the skin.
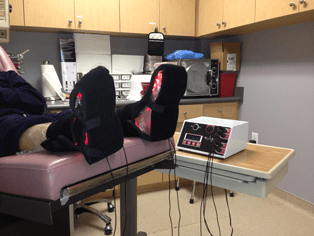
Treatment for peripheral neuropathy is medications, infra-red light therapy such as Anodyne which Dr. Fihman offers in her office and surgical nerve decompression.
- Vascular Disease
Vascular disease resulting from diabetes mellitus may be the underlying cause of most diabetes-related complications. Atherosclerosis which is a disease in which plaque builds up inside your arteries, which in time limits the flow of blood to your organs and other parts of your body. Decreased blood flow to the lower extremities causes poor healing and wounds become easily infected leading to gangrene and amputations. Peripheral arterial disease in diabetic patients occurs at a much younger age and with more rapid involvement than in nondiabetic patients. If ischemia is present the patient will be referred to a vascular surgeon who will perform an arterial bypass or an angioplasty. Dr. Fihman works closely with vascular surgeons in her area who strongly believe in limb salvage to help her have good results with these complicated cases.
Common diabetic foot complications
- Ulceration
Ulcers occur in diabetic patients as a result of peripheral neuropathy, peripheral arterial disease, or a combination of both. With chronic open wounds, the risk of osteomyelitis and amputation increases. Local wound factors such as infection, recurring trauma to a wound combined with a patient’s limited ability to sense pressure applied to it, continued pressure from a bony prominence, ischemia or a foreign body can cause wound healing to fail. Risk factors for ulceration include: poor glucose control, malnutrition, immunosuppressive drugs, steroids, tobacco, peripheral vascular disease and extremity swelling from venous insufficiency or congestive heart failure. Treatment for diabetic foot ulcers includes sharp debridement of all unhealthy tissue, off-loading the pressure that is causing the ulcer and applying various wound dressings. Sometimes surgery is required to remove pressure on the affected area by shaving, excising bone or correcting deformities such as bunions or hammertoes.
- Foot Infections
Diabetic foot infections are often polymicrobial meaning they have multiple types of bacteria. Diabetic foot infections that do not threaten the limb can be treated with either oral or IV antibiotics. Limb-threatening and life-threatening infections are treated with IV antibiotics. Antibiotics used to treat osteomyelitis, which is a bone infection may be taken for 4 to 6 weeks depending on the bacterial agent and the extent of the bony debridement. Osteomyelitis develops due to a non-healing or neglected ulcer. Due to diabetic neuropathy a patient with a foot infection such as osteomyelitis may not have any symptoms except an ulcer that is becoming worse or not healing. Foot infections are diagnosed by blood tests, x-rays, MRI, bone biopsy and cultures that will determine the correct antibiotic treatment.